The diagnosis of urticarial vasculitis is based on a comprehensive assessment of a series of clinical manifestations and auxiliary examinations. Urticarial vasculitis is a disease characterized primarily by urticaria-like skin lesions. Its diagnosis requires ruling out other similar conditions and confirmation through specific diagnostic methods.

Diagnosing urticarial vasculitis begins with a detailed medical history and observation of the patient's clinical presentation. The doctor will look for recurring skin erythema, papules, or vesicles; these lesions usually disappear within hours but reappear in other areas. The doctor will also inquire about fever, joint pain, or other systemic symptoms, as these may indicate the severity of the condition.
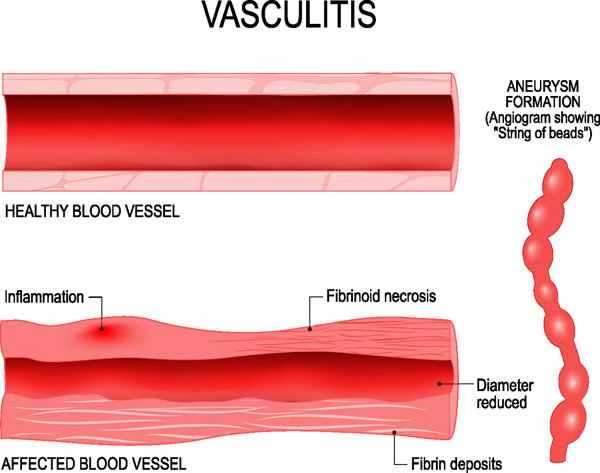
In addition to clinical manifestations, a definitive diagnosis of urticarial vasculitis requires further confirmation through several auxiliary examinations. Commonly used methods include blood tests and skin biopsies. Blood tests can assess inflammatory markers such as C-reactive protein and erythrocyte sedimentation rate; elevated levels of these markers may indicate the presence of inflammation. Skin biopsies involve taking a small piece of skin tissue for microscopic examination to observe for characteristic changes of vasculitis, such as perivascular inflammatory cell infiltration.

[Management Tip:]
1. Have regular blood tests to monitor inflammatory markers.
2. Avoid known allergens and irritants to reduce the risk of developing the disease.
3. If persistent or worsening skin symptoms occur, seek medical attention promptly.


